An EU-supported research project has shown significant progress in integrating advances in optical imaging and medical technology towards delivering faster diagnosis and treatment of bowel cancer the number two cause of cancer deaths.
Called PROSCOPE, the EU-wide consortium has demonstrated how multiple optical imaging methods can be used to enable doctors conducting colonoscopies to rapidly diagnose and therefore treat cancerous polyps in all sections of the bowel. Key elements of this work are now proceeding to in vivo testing.
In Europe, 160,000 people die each year from bowel cancer and both the EU and national governments have set tackling this through screening efforts as a priority public health goal.
At present when a doctor finds a polyp while screening there is no method available to tell them in real time if the polyp is cancerous. This leads to delays or even missed diagnoses. Looking for ways to deliver real-time diagnosis during colonoscopies is the radical objective of the PROSCOPE project.
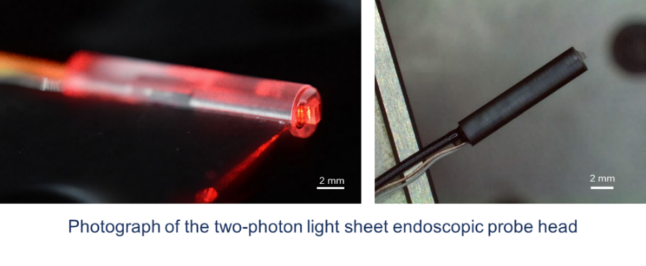
In addition to the traditional white light camera in current endoscopes, PROSCOPE has targeted adapting optical coherence tomography (OCT), multi-photon microscopy and Raman spectroscopy to provide the relevant biomarkers to the clinician during the imaging session. This has required both demonstrating the ability to identify and grade cancerous polyps as well as delivering this within a flexible endoscope which can reach all parts of the bowel.

Discussing the achievements of the project’s researchers, coordinator Dr. Peter E. Andersen, Technical University of Denmark, said: “Our ultimate objective is what has been called the Google Earth of colonoscopes: with the ability to zoom in at ever greater detail to find, examine and, if necessary, remove cancerous polyps.”
“Conventional white light can help the clinician to see an area of interest. Next, we zoom in to the depth of the lesion using first OCT, then multiphoton microscopy for critical metabolic information and finally Raman spectroscopy for molecular specific information to assess the lesion.”
Dr. Andersen said that the project’s researchers had been successful in a range of areas and that the new imaging platform can deliver the required diagnostic information and is now proceeding to in-vivo testing.
“We are particularly happy that the project has already led to new endoscopy and imaging products which are either in market or close to market. These include one product (the ArgoCap® by Ovesco) for the thermal ablation of tissue, which has been awarded ‘Innovation of the Year” by the European Society of Gastrointestinal Endoscopy.”
Dr. Andersen said that development of the concept will continue between the academic and industry partners who make up the consortium.